Chronic Kidney Disease (CKD) vs. Acute Kidney Injury (AKI): What’s the Difference?

Understanding the differences can lead to timely and effective treatment.
The kidneys act as the body’s natural filtration system, removing waste products, electrolytes, and excess fluid from the blood. When the kidneys fail to function properly, it affects multiple organ systems and can become life-threatening.
What is Kidney Failure?
Kidney failure refers to a condition in which the kidneys lose their ability to filter waste products from the blood. This leads to imbalances in fluid, electrolytes, and minerals in the body, which disrupts normal physiological functions. Without proper and timely treatment, kidney failure can result in severe complications and even death.
Chronic Kidney Disease (CKD)
Chronic Kidney Disease is characterized by a slow, progressive decline in kidney function over a long period of time. As the kidneys lose efficiency in filtering waste and toxins from the blood, the condition may progress to End-Stage Renal Disease (ESRD), requiring dialysis or kidney transplantation.
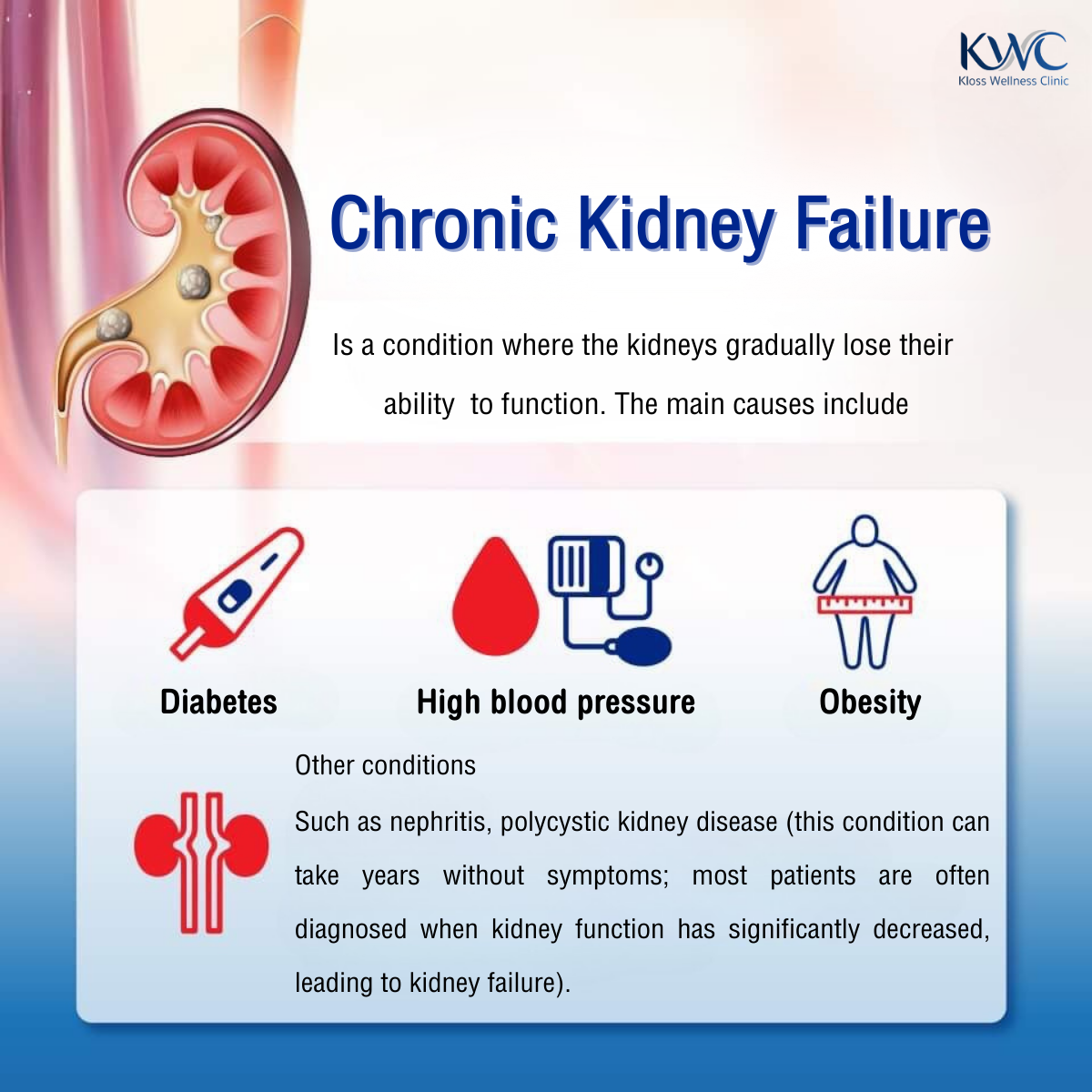
Causes of CKD
- Diabetes – the leading cause of CKD; high blood sugar damages the kidney’s filtering units.
- Hypertension (High Blood Pressure) – damages small blood vessels in the kidneys, impairing filtration.
- Glomerulonephritis – inflammation of the kidney’s filtering units.
- Polycystic Kidney Disease – a genetic condition causing cyst formation and loss of kidney function.
- Chronic urinary tract conditions – long-term obstruction or recurrent infections.
Symptoms of CKD
- Fatigue
- Frequent urination, especially at night
- Swelling of ankles or around the eyes
- High blood pressure
- Nausea, poor appetite, generalized itching
Diagnosis of CKD
- Blood tests – measurement of serum creatinine and estimated glomerular filtration rate (eGFR).
- Urine tests – detection of protein or other indicators of kidney damage.
- Imaging – ultrasound or CT scan to assess kidney structure.
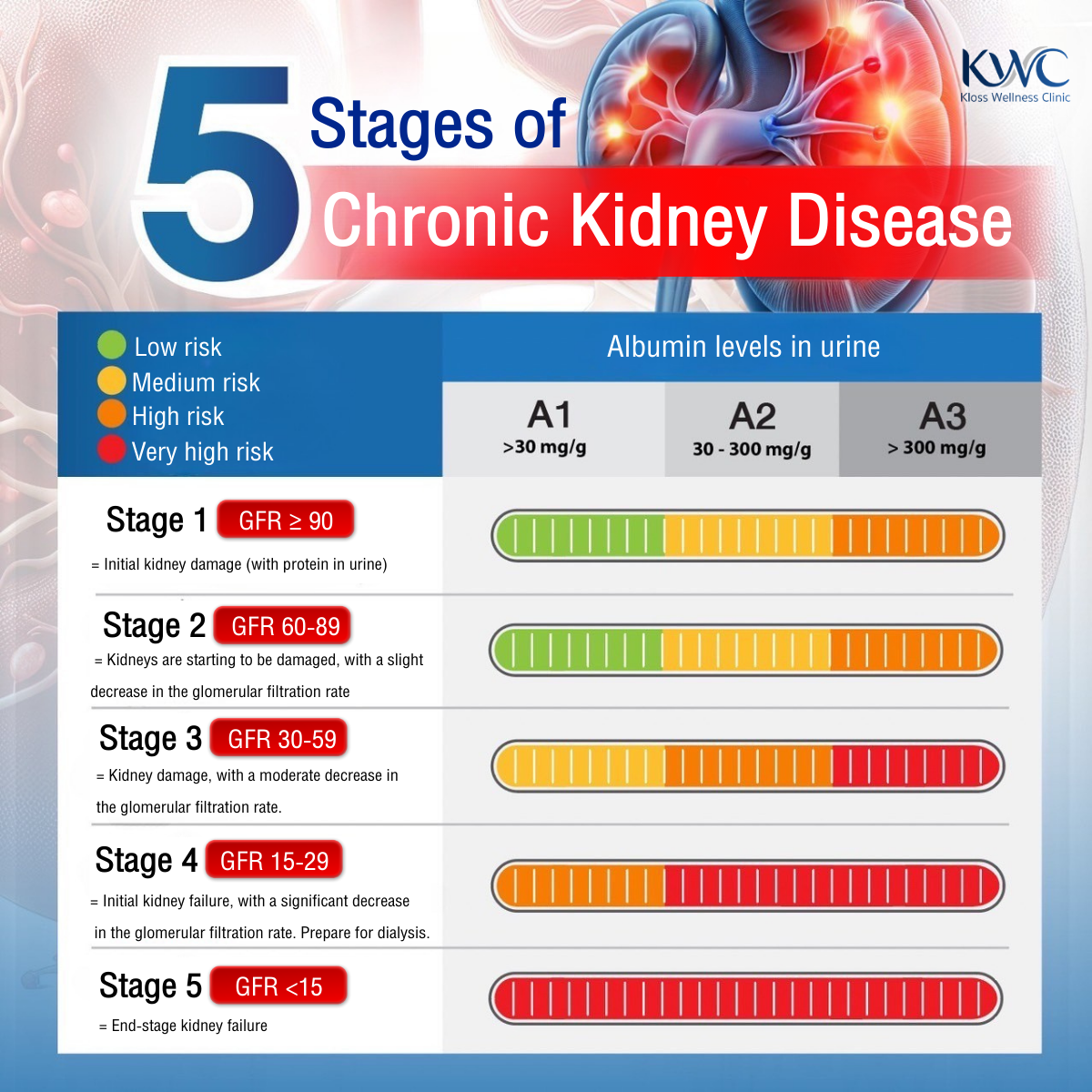
Stages of CKD (based on eGFR)
- Stage 1: eGFR ≥ 90 mL/min/1.73 m² – normal kidney function with evidence of damage.
- Stage 2: eGFR 60–89 mL/min/1.73 m² – mild decline in function with evidence of damage.
- Stage 3: eGFR 30–59 mL/min/1.73 m² – moderate decline in function.
- Stage 4: eGFR 15–29 mL/min/1.73 m² – severe decline in function.
- Stage 5: eGFR < 15 mL/min/1.73 m² – kidney failure, requiring dialysis or transplantation.
Acute Kidney Injury (AKI)
Acute Kidney Injury is a sudden decline in kidney function occurring within days to weeks. The kidneys fail to filter waste products efficiently, which can rapidly become life-threatening if not treated promptly and appropriately.
Causes of AKI
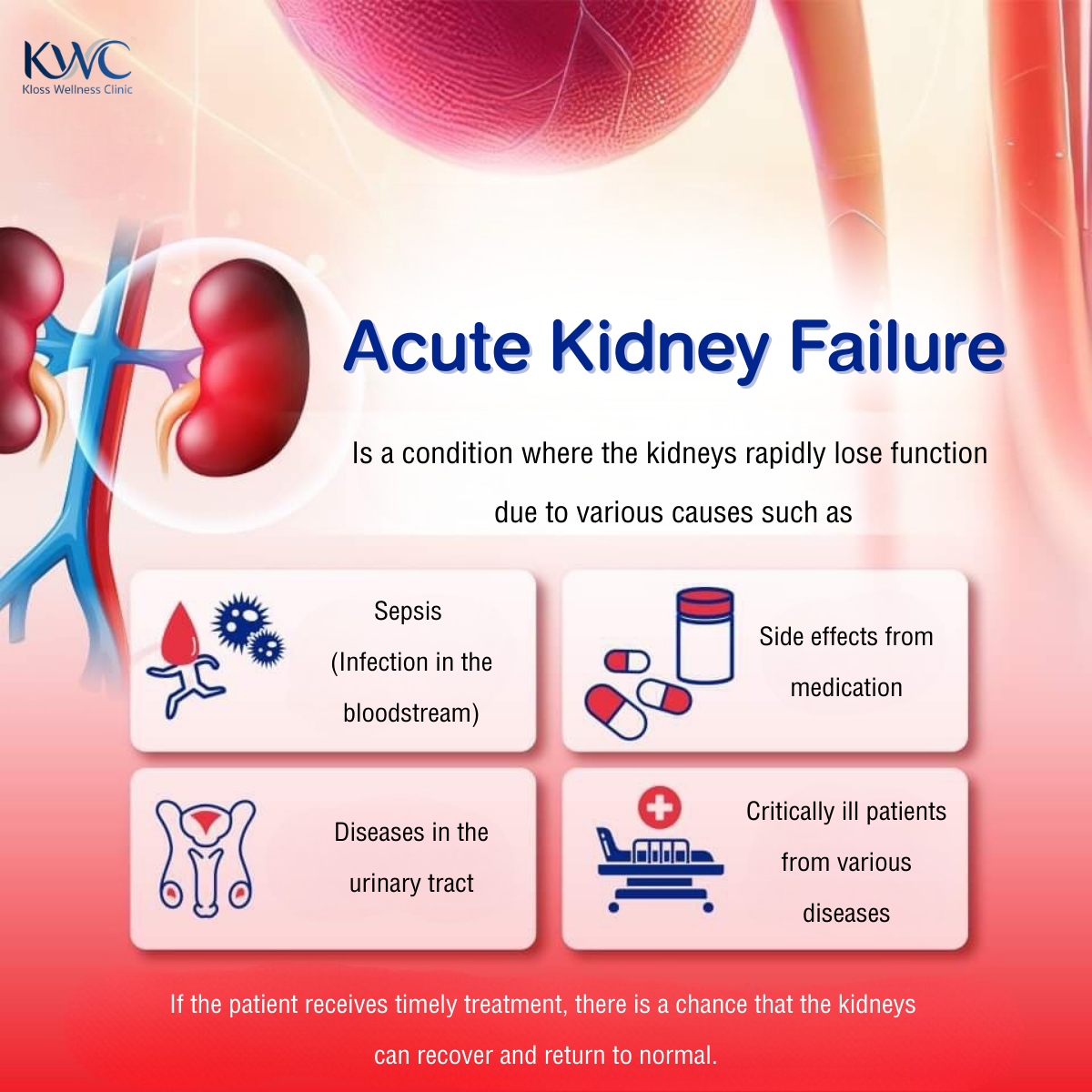
Reduced blood flow to the kidneys:
- Severe blood loss
- Severe dehydration
- Shock
- Heart failure
Direct kidney damage:
- Nephrotoxic drugs or chemicals (e.g., certain antibiotics, NSAIDs)
- Severe infections (sepsis)
- Renal vein thrombosis
- Acute glomerulonephritis
Urinary tract obstruction:
- Kidney stones
- Tumors or cysts obstructing the urinary tract
- Ureteral stricture
Symptoms of AKI
- Reduced urine output or complete absence of urination
- Swelling of legs, ankles, or around the eyes
- Shortness of breath, fatigue
- Nausea, vomiting
- Confusion or loss of consciousness
- Abnormally high or low blood pressure
Diagnosis of AKI
- Blood tests – serum creatinine and eGFR levels.
- Urine tests – detection of protein, blood, or other abnormalities.
- Imaging – ultrasound, CT scan, or MRI to assess structure and detect obstruction.
- Kidney biopsy – in select cases, to determine the underlying cause.
Key Differences Between CKD and AKI
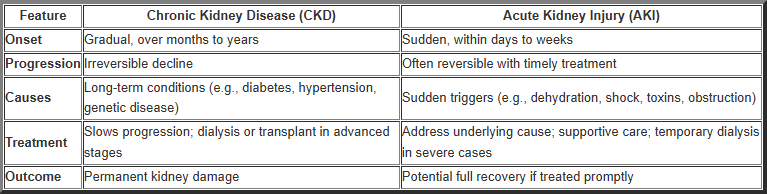
Conclusion
- CKD: develops gradually, causes irreversible loss of function, and requires long-term management.
- AKI: occurs suddenly, but kidney function may recover if treated promptly.
Understanding the differences between CKD and AKI is essential for accurate diagnosis, timely intervention, and effective patient care.
Translated and compiled by ArokaGO Content Team
If you would like professional consultation and kidney care, you can visit Kloss Wellness Clinic:
✓ Expert care by experienced physicians
✓ Thorough analysis and personalized treatment
✓ Safe procedures with international-standard equipment
✓ Services delivered with quality, honesty, and responsibility
Book your health consultation at Kloss Wellness Clinic (3 branches):
-
Serithai Branch: 099-265-2495
-
Muang Thong Thani Branch: 099-246-3691
-
Bangna Branch: 095-636-2326
-
LINE ID: @klosswellness
-
Web Site: Kloss Wellness Clinic
Kloss Wellness Clinic
Share this article
More Articles
Discover more insights on health care and medical tourism.
The Importance of Vitamin K in Osteoporosis
Osteoporosis is a major public health problem, comparable to diabetes, hypertension, and hyperlipidemia. It has long posed a serious threat to the health and quality of life of the Thai population, particularly older adults. Most elderly individuals with osteoporosis experience no warning symptoms or early signs, resulting in delayed diagnosis and lack of early treatment. Consequently, these individuals are at high risk of fragility fractures at various sites, including the wrist, spine, hip, and upper arm.
Tennis Elbow: Elbow Pain That Doesn’t Affect Only Athletes
Tennis Elbow, medically known as Lateral Epicondylitis, is an inflammatory condition of the tendons on the outer side of the elbow. It is caused by repetitive use of the arm, wrist, or elbow over a prolonged period, such as typing on a computer, using a smartphone, lifting heavy objects, or even doing routine household chores.

List of Private Hospitals in Thailand
Thailand is widely recognised as one of Asia’s leading destinations for private healthcare, offering international-standard medical services, advanced technology, and highly experienced physicians. Private hospitals in Thailand serve both local residents and international patients, particularly in areas such as complex surgery, health check-ups, wellness, and medical tourism.